The pain is burning in nature, but can also be deep and dull. Decreased sensitivity is usually minimal or absent. Sometimes there is hyperesthesia. Against the background of pain syndrome, paresis and atrophy of the anterior muscles of the thigh occur. The pain usually resolves within a few weeks but sometimes lasts for several months. Paresis and atrophy persist for many months, sometimes accompanied by unexplained weight loss, which often raises the suspicion of a malignant tumor.
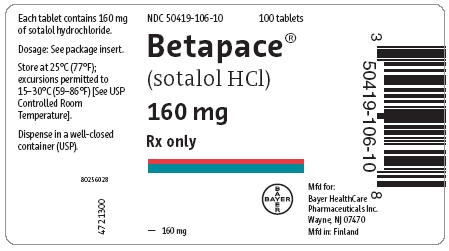
These two conditions can only be distinguished by electromyography, which reveals denervation changes in the paravertebral muscles in radiculopathy, but not in plexopathy. At many patients manifestations of a distal symmetric polyneuropathy are at the same time noted. Even in severe cases, the prognosis is favorable, but recovery can take from several months to several years, and in some patients the residual defect remains. The differential diagnosis has to be carried out with ischemia of the thigh muscles due to order betapace, which sometimes occurs in severe diabetes mellitus and is manifested by acute pain, local tenderness and edema. The quadriceps, abductors, and biceps femoris are particularly commonly affected.
Thoracoabdominal neuropathy. The result of the defeat of the lower thoracic roots Th6-Th2. Clinically, a lesion of one or two adjacent roots is usually detected. Sometimes the symptomatology is bilateral and is accompanied by signs of damage to the upper lumbar roots. Sometimes such patients are even subjected to surgery (especially often cholecystectomy). The study reveals hypesthesia or hyperesthesia in the corresponding dermatomes. At the same time, motor fibers are also affected, but more often it occurs subclinically. With the involvement of several adjacent roots innervating the muscles of the abdominal wall, the formation of an abdominal hernia is possible.
Denervation of the paravertebral muscles on EMG indicates damage to the root or nerve. The pain usually resolves within a few days, while the sensory disturbance regresses within 4-6 weeks. Even less often, diabetic radiculopathy affects the cervical roots, of which C5-C7 is more often involved, sometimes on both sides. Radiculopathy often recurs, changing localization. Sometimes the roots are simultaneously affected at several levels (polyradiculopathy).
Cases of lower lumbar or cervical radiculopathy can be difficult to buy sotalol online from vertebrogenic pathology. It should be borne in mind that with diabetic radiculopathy, the vertebral syndrome is mild (limited mobility of the spine, tension of the paravertebral muscles, scoliosis), the pain does not decrease in the supine position and intensifies at night. Changes detected by radiography are nonspecific and do not allow differentiating diabetic radiculopathy from vertebrogenic.
Betapace pills over the counter
- Multiple mononeuropathy. It is manifested by acute ischemic damage to individual nerves, simultaneous or sequential.
On examination, limited mobility of the eyeball is revealed with preserved pupillary reactions. This is due to the fact that during ischemia, the central fibers of the nerve suffer, while the parasympathetic fibers located along the periphery remain intact (when the nerve is compressed, for example, by an aneurysm of the posterior communicating artery, the first symptom is usually dilated pupil). The prognosis is favorable, full recovery within 3-6 months is the rule, but sometimes it is somewhat delayed. In some cases, cranial neuropathies recur.
In this case, the oculomotor (III) nerve is especially often involved, less often the abducens (VI) and trochlear (IV) nerves (acute diabetic ophthalmoplegia). It usually affects people over 59 years of age. The disease begins acutely with intense pain in the periorbital region, which precedes weakness by several days.
- Since neurological disorders may be the first manifestation of diabetes mellitus, the study of betapace pills glucose levels should be included in the complex of examinations in any patient with PNS damage.
Therefore, diabetic neuropathy should be diagnosed only when other diseases that can cause similar symptoms have been excluded. A family history of sotalol and the presence of a cavus foot may supportIn other polyneuropathies, an acute onset and a significant increase in protein content in the CSF are more characteristic of Guillain-Barr� syndrome, and the detection of a paraprotein in the blood serum is in favor of primary amyloidosis, multiple myeloma, or benign gammopathy.
On the other hand, one should be warned against uncritical attribution of any neurological pathology in a patient with diabetes mellitus to this disease. Thoracic radiculopathy requires a differential diagnosis with diseases of the abdominal cavity, tuberculous spondylitis, metastatic lesions of the spine, etc. Lumbar puncture and CSF examination are performed in order to exclude Guillain-Barr� syndrome or meningeal carcinomatosis.
Normalization of blood sugar levels is the main condition for the stabilization and regression of the manifestations of diabetic neuropathy. However, there is currently no evidence that switching from oral antidiabetic agents to insulin accelerates recovery in diabetic neuropathy. Improvement is recorded no earlier than 6 months after stabilization of glycemia.
Protein levels in the CSF in diabetic neuropathy are often elevated but rarely exceed 1.0 g/l. In multiple mononeuropathy, the differential diagnosis with vasculitis is important. The effectiveness of aldose reductase inhibitors (albrestatin, tolrestat), as well as gangliosides and complex sialoglycolipids stimulating axonal regeneration, is being studied, but at present these drugs cannot be recommended for widespread use. Data on the effectiveness of the myoinositol-restricted diet are conflicting. The role of immunotherapy in symmetrical proximal motor neuropathy remains unclear.
order betapace 40mg online
Symptomatic therapy is important. With persistent burning pain, in addition to analgesics and NSAIDs, tricyclic or tetracyclic antidepressants (amitriptyline, nortriptyline, desipramine or mianserin) are used. With poor tolerance of these drugs, serotonin reuptake inhibitors are used. It should be borne in mind that the analgesic effect of antidepressants is sometimes more pronounced when prescribing small or medium doses. With shooting pains, anticonvulsants, especially carbamazepine, are sometimes effective. Difenin inhibits the secretion of insulin, and therefore should be avoided taking this drug.
It is possible to add neuroleptics to antidepressants, but one should remember about the risk of developing neuroleptic syndrome. To reduce pain, mexiletin, clonazepam, clonidine, and external preparations of capsicum (capsaicin) are also used.
With the ineffectiveness of non-drug measures, fludrocortisone, midodrine or dihydroergotamine are prescribed, NSAIDs, sometimes r-blockers (pindolol) are used as adjuvants. With difficulty urinating, it is recommended to empty it regularly (every 34 hours), cholinomimetics and a-blockers. For delayed gastric emptying, metoclopramide, domperidone, low doses of erythromycin are indicated; for diarrhea, low doses of sotalol (eg, tetracycline), loperamide, or codeine phosphate are indicated.